Decoding the Updated CDC Guidelines for Omicron
By fighting against this pandemic for more than two years, it is apparent that the COVID-19 virus is going to be with all of us for much more time than most of us initially thought. This is because new variants continue to emerge due to mutations in the viral sequence of SARS-CoV-2. Although rich and developed countries have adequate vaccines, several developing countries still do not have access to these life-saving measures. Unless and until we have global equity in vaccinations, the viral mutations continue to occur and, unfortunately, new variants continue to emerge.
One of the new variants spreading globally is ‘Omicron’. Here are some common questions that I get from patients and my response to them.
Q: How is the ‘Omicron’ variant different from the ‘Delta’ Variant?
Viruses are known to change and adapt to newer environments by changing their own genetic sequences. Some of the viruses persist and some don’t. The well-known Delta variant, also known as B.1.617.2, was first identified in India. It was specifically known to spread faster than the previous variants, causing severe illnesses and mortality. Currently available vaccines are effective in preventing infections and monoclonal antibody treatments such as Bamlanivimab, Casirivimab, etc are effective against the Delta variant.
The Omicron variant, also known as B.1.1.529, was first detected in South Africa in November 2021. It is known to be highly infectious and spreads even faster than the Delta variant. The preliminary data suggest that some monoclonal antibody treatments may not be as effective against infection with Omicron. Initial data also show that the infections with the Omicron variant may not be as severe as infections with the Delta variant. Omicron is currently causing another huge wave of infections in the United States and around the globe. It is estimated to peak by late January 2022.
Q: How long one should quarantine or isolate? Can you clarify the updated CDC guidelines?
-
Isolation guidance after being tested positive:
Isolation for at least five days from the onset of symptoms is recommended. Please remember, the onset of symptoms is considered as day zero. Day one is the first full day after your symptoms develop.
Isolation can be ended after five days of symptom onset and if your symptoms have improved with no fever for more than 24 hours (without the assistance of fever-reducing medications). Some symptoms like loss of taste and smell may take longer to improve and don’t apply with this guide.
Wearing a mask, however, needs to be continued at home and the workplace even after the isolation period ends for at least 10 days after the onset of symptoms.
-
Quarantine guidelines after exposure to a person with COVID-19 infection:
You need to quarantine if you are at least 18 years or older and exposed to COVID-19 patients. If you have not completed the primary vaccination series, or have not received a booster shot, quarantine is more than necessary.
Quarantine at home for at least five days from the time of last exposure to a patient with COVID-19. Watch for any symptoms of COVID-19 during the quarantine period and five days following the quarantine period. If you develop any symptoms suggestive of COVID-19, get tested immediately. You should get tested five days from the time of last exposure, even if you do not develop symptoms.
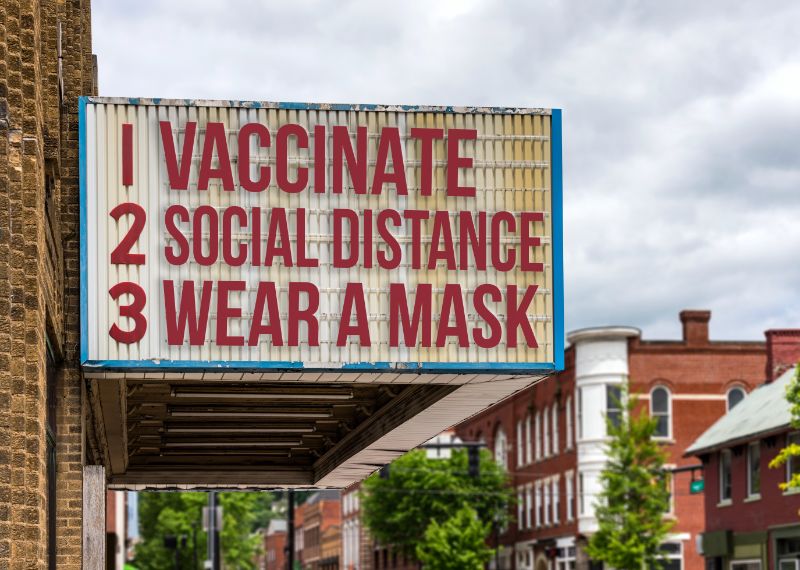
Q: What things can we do to curb the spread of new variants?
Masks continue to be an effective way to curb the community spread of newer variants. Available data suggest that getting the booster shot for COVID-19 prevents severe illness by the virus. Evidence concerning the Omicron variant is limited at this time.
Q: What treatment options are available at this time if we get infected?
In a randomized control study, Pfizer’s Paxlovid (nirmatrelvir tablets and ritonavir tablets) has been effective in decreasing COVID-19 related hospitalization or death by 88% compared to the placebo when taken within five days of symptom onset.
On December 22nd, 2021, the US Food and Drug Administration issued an emergency use authorization for Paxlovid in the treatment of mild-to-moderate COVID-19, in both adults and pediatric patients (12 years or more of age), who are at high risk of hospitalization or death. These tablets should be started within five days of symptom onset, preferably as soon as possible. The availability of these tablets is limited as of now.