As the BA.2 Variant Gets Aggressive, Doctors Resonate on Getting COVID Vaccines, Staying Current on All Doses
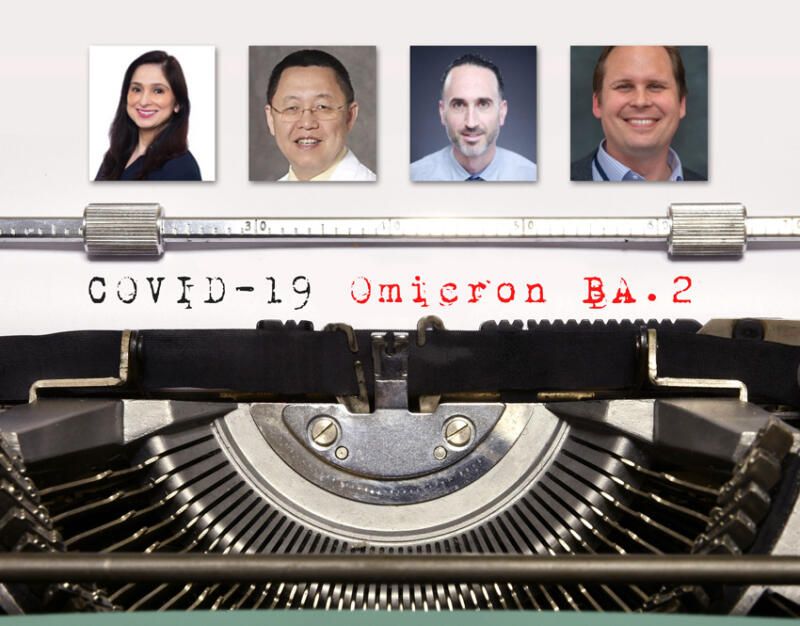
(Above, Inset l-r): Dr. Manisha Newaskar, Pediatric Pulmonologist, Stanford Children’s Health; Dr. Dali Fan, Health Sciences Clinical Professor, UC Davis; Dr. Daniel Turner-Lloveras, co-founder, Latino Coalition Against Covid-19 and a volunteer physician for the Covid-19 Vaccine Education & Empowerment in Detention program; Dr. Ben Neuman, Professor of Biology and Chief Virologist of the Global Health Research Complex, Texas A&M University. (Siliconeer/EMS/Shutterstock)
According to Sandy Close, EMS director, BA.2 variant now accounts for half of new COVID infections in New York and New England and close to 35% in California and elsewhere. Experts – Dr. Manisha Newaskar, Pediatric Pulmonologist, Stanford Children’s Health; Dr. Dali Fan, Health Sciences Clinical Professor, UC Davis; Dr. Daniel Turner-Lloveras, co-founder, Latino Coalition Against Covid-19; and Dr. Ben Neuman, Professor of Biology and Chief Virologist of the Global Health Research Complex, Texas A&M University – shared their thoughts on what does this means for the future; who’s most at risk; will a second booster mitigate the impact; what do we do about masks; how about children, especially those under five, who are not yet eligible for vaccines? Here is a recap of the briefing held April 8.
How did the BA.2 variant emerge and can you compare its characteristics to that of its predecessors, Omicron and Delta, and can we expect to see a new wave of infections?
Dr. Neuman: BA.2 is a very similar virus to Omicron and it probably shares a common ancestor with this but this is a common ancestor whose name we do not know. It is likely that if we had monitoring in whatever part of the world this came from, we would have called this a particular Greek letter variant but it most likely happened out of the site of our sequencing.
I think the most important place that BA.2 and Omicron came from is from a person and it’s most likely a person who either couldn’t or didn’t have a vaccine, and this is something that may have happened in Africa. I don’t think it’s important to put a place on it so much as a cause because when we vaccinate people we can essentially stop this from happening. I like the progress that has been going on in that but there’s still a lot of work to do for sure.
As the virus grows, it changes. Change is part of the growth of coronaviruses and many other viruses, so it’s certain and what we have seen so far is that the virus, for a while, was getting faster, it was just better at jumping from one person to another. I think of this like the old story of the tortoise and the hare. The early variants were like the hare, they ran very fast and very far, as the climate became more difficult for viruses, as we built up more immunity through vaccination and through repeated exposure, it became impossible for viruses like this to grow and we’ve recently seen that the Delta variant which is the last of these early viruses has effectively gone extinct worldwide.
It is only the tortoises that are left and viruses like BA.2 and Omicron, think of them as being armored. They’re not particularly fast although they can spread in new ways. These are the viruses that can spread to people who have some immunity already and that’s the concern these represent a possibility of repeated exposure and additional bad things happening even when people have taken some of the right precautions. Omicron is not our friend, it’s not anyone’s friend, and it’s something that we need to get rid of as quickly as possible in my opinion as a virologist.
Hong Kong and China are being very badly hit by Omicron and BA.2. We’re seeing surges across Europe that are driven by Omicron and BA.2.
A lot of the concerns about vaccines have been that they don’t work against some of the other variants. You can either vaccinate against Omicron or something else, and biology has perhaps thankfully simplified the picture because now there are only Omicron-like viruses, and I think it points us a clear path forward which is making more Omicron-like vaccines which can be more effective because their limitations are no longer a limitation if the other strains are extinct.
Commenting on Dr Anthony Fauci’s statement last month, in which he said that the U.S. is not likely to be hit as hard as the UK and Europe, Dr Neuman said, “Yes, I think that has come to pass more or less, but I don’t think it’s because we necessarily did anything right between Thanksgiving and Valentine’s Day. We had a minimum of 10 percent of the U.S. population infected with some version of COVID and most likely the number is higher, it’s probably closer to one in four people, that were infected.
All he’s saying is that the viruses kind of burn out the easy fuel for the moment but I think the problem with dealing with things like this is complacency. The immunity that we build to exposures or vaccines is temporary. It has a window. It’s like a little egg timer and it ticks down, one tick at a time, until you’re no longer protected and there is no way to tell from looking at a person whether they will be protected against this variant or the next variant and as time goes on it becomes less likely that protection that we have from whatever means will actually stand up against the new variants that’s just natural selection. It’s a powerful way of finding solutions to problems and the virus is changing because we are putting it in a bad spot forcing it to change. I see a lot of progress but we are definitely not done yet.”
As practicing physicians what are you seeing at the hospital and who remains most at risk for hospitalization and death from COVID?
Dr. Fan: The caseload for our hospital has not risen yet. We had nine patients total admitted to the hospital for COVID positive back a few months ago, our peak was 142.
The newest wave has not hit the hospital yet (as of April 8).
The most vulnerable can be classified in three different ways – one is the vaccinated versus the unvaccinated, the vaccinated ones are more protected and then the unvaccinated ones are the most vulnerable. How far away from inoculation of the vaccine is the second factor if your dose or your booster dose is further away, the immunity of protection might have weaned off; and the third one is a general vulnerability, if the caseload in the community is higher, then everybody’s vulnerability is higher.
According to the CDC, by April 2, 2022, BA.2 has become the dominant strain in the U.S.
Are you experiencing fresh wave of pediatric infections and could you discuss the impact of the BA.2 variant on younger children, the majority of whom remain unvaccinated?
Dr. Newaskar: We are not seeing an increase in number of cases in the hospitals in fact in last few weeks there is a decline in the number of patients that we have seen getting hospitalized.
It seems like there are still some infections going on in the community but it’s not to the extent that we were seeing back in January-February time frame. What’s coming up is unknown and we need to be uh prepared for that.
In terms of vulnerability, we look it as vaccinated versus unvaccinated. In the previous surges, it was very clear, especially also in pediatric population, that children who were unvaccinated were at much higher risk for getting hospitalized compared to the vaccinated ones. Vaccination does protect you from severe infection especially hospital admission, ICU and ventilator dependence, vaccination is the key.
There are other vulnerable population, especially in kids, children who are immunocompromised, who are undergoing cancer chemotherapy, or have some other types of diseases where they can’t mount immune response. Obesity, uncontrolled asthma, those are the population I am always worried about because over time we have seen that these are the patients that have been hit the most and so taking care of your underlying medical condition is important and getting vaccinated.
This is it’s becoming sort of endemic now and new waves are expected to come. Our job is to protect ourselves, our family, and community by doing the right thing, which is getting vaccinated.
Latinos make up 40 of the population in California and yet looking at recent data from the California Department of Public Health, they account for 47 percent of hospitalizations and 43 percent of debts from COVID-19. Could you explain what is happening here and will the BA.2 variant further skew those numbers?
Dr. Daniel Turner-Lloveras: The data has been very consistent for the last two years when it comes to the Latino population, which has borne the brunt of this pandemic. If you look at the numbers, Latinos make up 38.9-40 percent of California’s population but 40 percent of its confirmed COVID infections and 44 percent of recovery. By contrast non-Latino whites represent 36 percent of the state population and are 24 percent of confirmed cases and 34 percent of COVID deaths.
Similar disparities exist in vaccinations in the state. Only 64 percent of Latinos have received at least one COVID vaccine dose and right from the beginning of this pandemic research found Latinos have overrepresented in the frontline occupations which are associated with higher risk of infection through more frequent exposure to the virus. Latinos are more likely than non-latino whites to live in overcrowded housing that is unsuitable for proper quarantine isolation, and there’s the lack of access to health care. This has been an ongoing problem. Eligibility for health insurance made it hard to test treat vaccinate people at the height of the pandemic even when there was government funding that provided COVID testing and vaccines for uninsured and undocumented.
Would you recommend getting a second booster for people over 50?
The short answer is, yes.
“If you’re over the age of 60, it’s in your best interest to receive that vaccine. For under 50, the data is not as clear but if you’re over 60 or if you’re at high risk for whatever reason then it’s in your best interest to receive vaccines,” said Dr Neuman.